Understanding TMJ Dysfunction and Conservative Care Options
A structured, patient‑centred approach to jaw pain, tension, and TMJ‑related symptoms
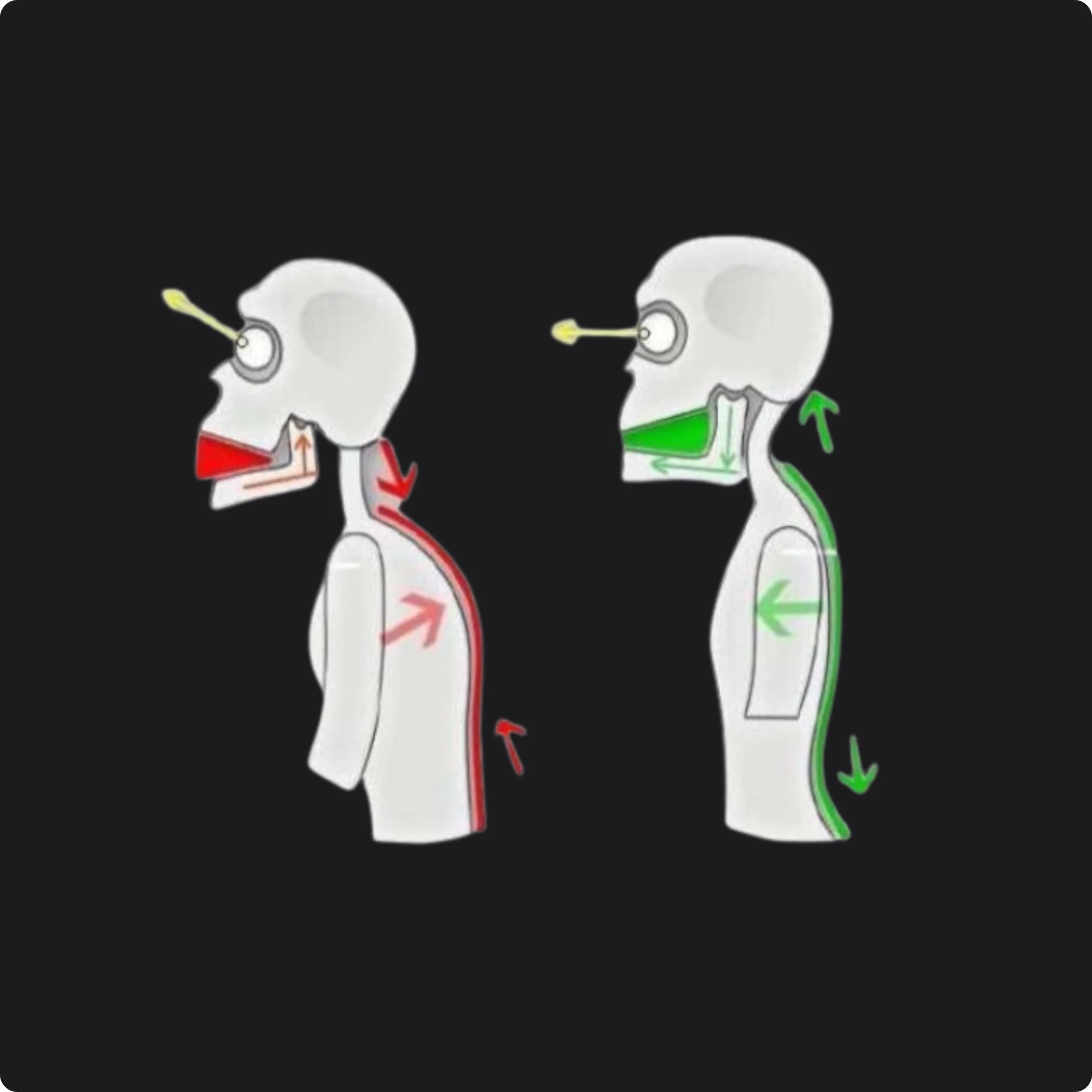
Jaw pain and TMD symptoms are rarely caused by a single issue in the jaw joint itself. For many people, symptoms develop from a combination of muscle overuse, habitual clenching, posture, breathing patterns, stress, and how the nervous system responds to load.
Conservative care focuses on reducing strain on and improving how it functions over time. My role is to help patients understand the “why”, and to support the muscles, movement patterns, and habits that influence symptoms.
The temporomandibular joints (TMJs) connect the lower jaw to the skull and are involved in chewing, speaking, swallowing, and yawning. TMJ dysfunction (often referred to as TMD or TMJD) occurs when these joints and the surrounding muscles are under excessive or poorly managed load.
Common symptoms include:
Jaw pain, stiffness, or fatigue
Clicking, popping, or restricted opening
Facial pain or pressure
Headaches, neck pain, or shoulder tension
Ear symptoms such as fullness, pressure, or ringing
Clenching or grinding (daytime or during sleep)
TMJ symptoms are often influenced by muscle tension, posture, airway and breathing patterns, and stress — which is why conservative, musculoskeletal‑based care can be helpful.
What Is TMJ Dysfunction?
What Does “Conservative Care” Mean for TMJ Symptoms?
Conservative care refers to non‑invasive, movement‑based approaches aimed at improving function, reducing strain, and supporting symptom management without surgery or irreversible procedures.
Rather than attempting to fix the jaw joint through permanent surgeries, conservative care focuses on:
Reducing excessive muscle tension
Strengthening muscles that have weakened
Improving jaw and neck mobility
Addressing contributing postural or breathing patterns
Supporting nervous system regulation
Helping patients better manage daily load on the jaw
This approach is often appropriate as a first‑line option and can also complement dental or medical care.
How I Support Patients With TMJ Dysfunction
“Care works best when it is individualized, structured, and progressive. My approach combines assessment, hands‑on therapy, education, habit modification and active rehabilitation to address the sources or root causes contributing to my patients symptoms”
Care begins with a detailed assessment that looks beyond the jaw alone. Depending on the individual, this may include:
Jaw and tongue movement quality and range of motion
Muscle tone and tenderness in the jaw, face, neck, and upper body
Posture and head‑neck positioning
Breathing patterns and resting jaw habits
Assessment for tethered oral tissues
The goal is to identify contributing patterns rather than focusing only on where pain is felt.
Thorough Assessment
Hands‑on treatment is used to help reduce excessive muscle tension and support healthier movement patterns.
This may involve work focused on:
Jaw, face and tongue muscles
Neck, shoulders, and upper back
Areas contributing to compensation or guarding
Techniques are selected based on comfort and clinical findings and may include soft tissue techniques and gentle nervous system‑calming approaches. Treatment is always adapted to the individual.
Time is also taken to show the patient how to provide themselves manual therapy in between appointments.
Targeted Manual Therapy
Myofunctional Exercises, Habit and Motor Retraining
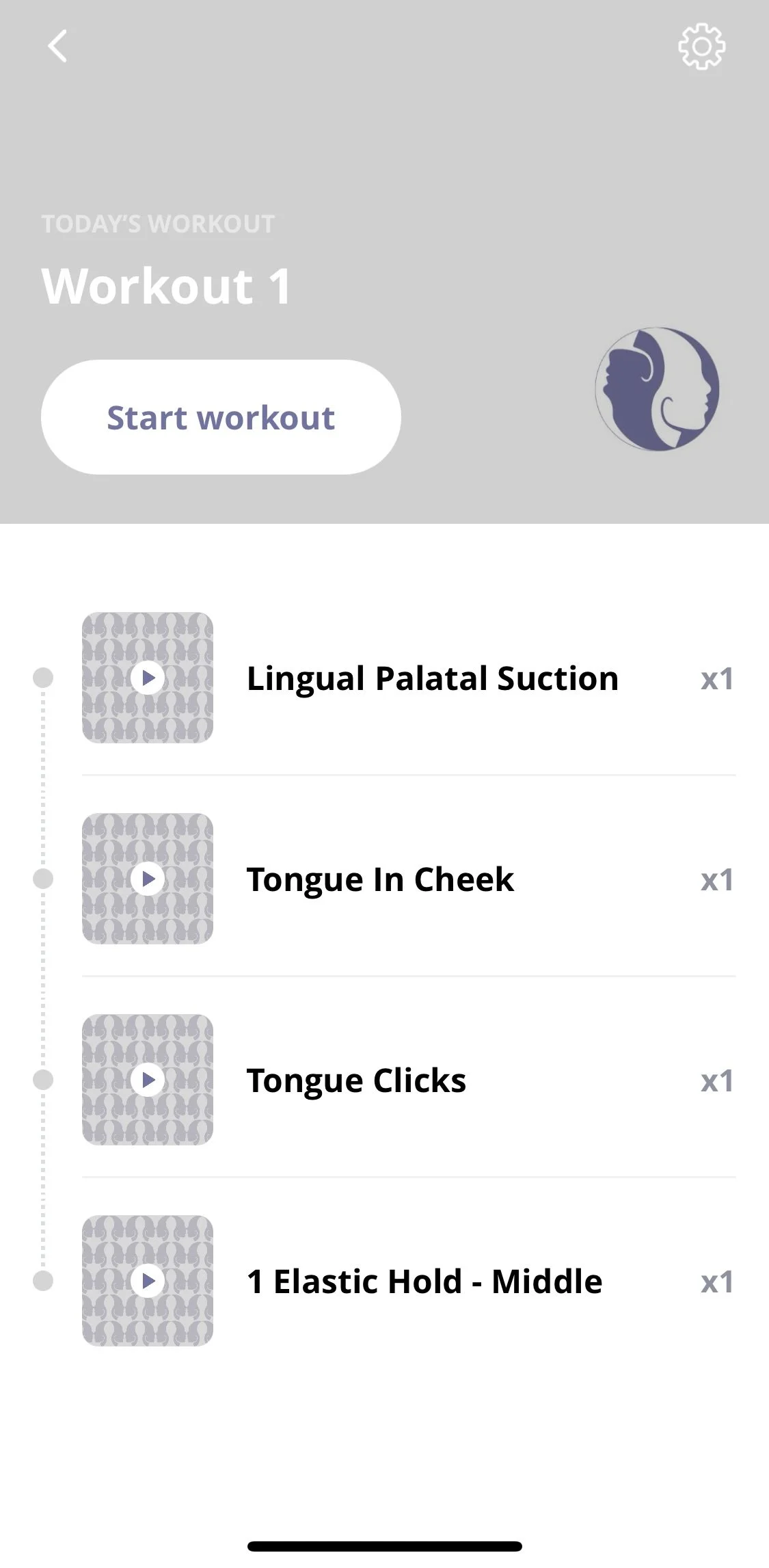
Hands‑on care alone is rarely enough to create lasting change. Active therapy helps retrain how our muscles function throughout daily life.
This may include:
Gentle jaw and tongue coordination and mobility exercises
Awareness of tongue posture and oral rest position
Breathing strategies to reduce tension
Habit modification related to clenching or jaw holding
Adjustment to sleep habits and nasal hygiene
These strategies aim to reduce repeated overload between appointments and support long‑term symptom management.
Education and Self‑Management Support
Education is a key part of conservative TMJ care. Understanding contributing factors can help patients feel more confident and in control of their symptoms.
Education may include:
What tends to aggravate TMJ symptoms
How posture, stress, and breathing influence jaw tension
Flare‑up management strategies
Pacing and symptom tracking guidance
Working Alongside Other Healthcare Providers
TMJ dysfunction care often benefits from a collaborative approach. Many patients are also under the care of dental professionals, physicians, or other regulated healthcare providers.
My role is to support the musculoskeletal and functional contributors to symptoms and to work within a conservative, team‑based model of care when appropriate.
If you are experiencing jaw pain or TMJD‑related symptoms, a structured assessment can help identify contributing factors and appropriate conservative care options.
Reach out to me or speak with your healthcare provider to determine whether conservative, musculoskeletal‑based care may be appropriate for you.
This information is provided for educational purposes and does not replace diagnosis or care from a physician or dentist.